Chronic Venous Insufficiency: A Comprehensive Guide
Chronic Venous Insufficiency (CVI) is a condition that affects millions of people worldwide. It occurs when the veins in the legs are unable to carry blood back to the heart effectively. As a result, blood pools in the legs, causing swelling, pain, and other uncomfortable symptoms. In this blog post, we will take you through everything you need to know about Chronic Venous Insufficiency – from its definition and prevalence to its impact on your health, causes, stages, diagnosis, treatment options, prevention tips, and day-to-day management. We will also answer one of the most commonly asked questions about CVI – can it be cured completely? If you or someone you know is suffering from CVI or wants to learn more about it for prevention purposes, keep reading!
Contents
- Chronic Venous Insufficiency Explained
- The Impact of Chronic Venous Insufficiency on Your Health
- Identifying the Signs and Causes of CVI
- Progression of Chronic Venous Insufficiency
- Diagnosing Chronic Venous Insufficiency
- Treatment Approaches for CVI
- Preventing Chronic Venous Insufficiency
- Living with Chronic Venous Insufficiency
- Can Chronic Venous Insufficiency be Cured Completely?
- Conclusion
Chronic Venous Insufficiency Explained
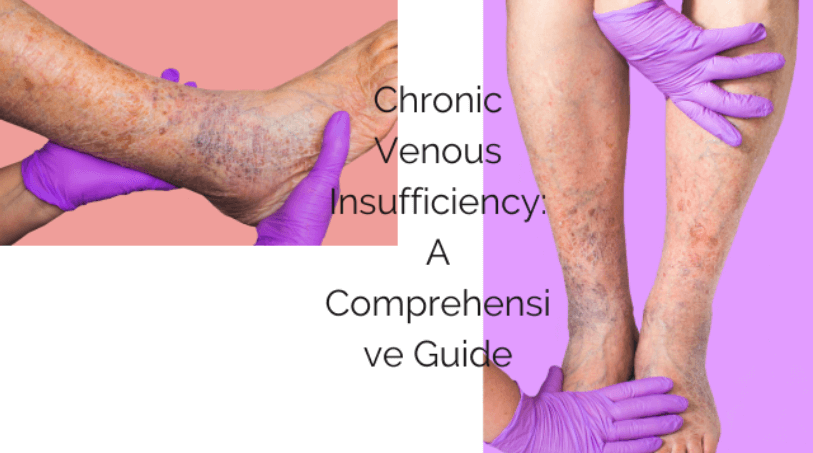
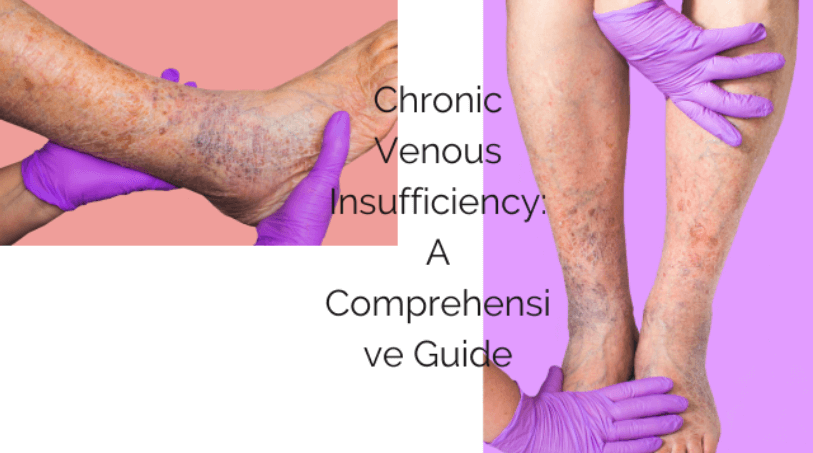
When the valves in the leg veins fail, blood may flow in the wrong direction, leading to chronic venous insufficiency (CVI). This can result in varicose veins, leg swelling, and skin changes, impacting quality of life. Identifying CVI is crucial for effective management as it may progress if left untreated, affecting overall health.
Definition of Chronic Venous Insufficiency
Chronic venous insufficiency occurs due to inadequate function in leg veins, leading to symptoms like leg swelling, pain, and skin changes. Damaged vein walls or malfunctioning valves can cause CVI, making early detection and proper diagnosis essential. This understanding is crucial for developing an effective treatment plan.
The Prevalence of Chronic Venous Insufficiency
Chronic venous insufficiency is a common condition, affecting a significant number of individuals worldwide. It is more prevalent in adults, especially those with a family history of venous disorders. The prevalence of CVI underscores the importance of raising awareness and early intervention. Lifestyle changes can play a key role in reducing the prevalence of chronic venous insufficiency. Awareness of the prevalence of CVI is important for promoting proactive measures for prevention.
The Impact of Chronic Venous Insufficiency on Your Health
Understanding the effects of CVI on health is crucial for early intervention and treatment. CVI can result in venous ulcers, skin changes, and prolonged discomfort. It may also elevate the risk of deep vein thrombosis and pulmonary embolism, emphasizing the need for comprehensive management strategies. Effective management can significantly enhance the overall health and well-being of individuals.
Understanding the effect of CVI on the body
CVI affects the lower leg, leading to symptoms like swelling and skin changes, emphasizing the need for timely medical intervention. It may cause chronic venous stasis ulcers, impacting mobility and necessitating personalized treatment plans. Proper management can enhance the overall quality of life for those affected, aligning with the main goal of NLP in healthcare.
Identifying the Signs and Causes of CVI
Recognizing indications is essential for early intervention. Symptoms include leg swelling, aching, and varicose veins. Identifying signs can prompt medical treatment. Causes may involve obesity, family history, and prolonged standing. Early recognition leads to preventive measures.
Recognizing the Symptoms of CVI
Symptoms of chronic venous insufficiency like leg swelling, heaviness, and discomfort are often observed. Skin changes such as discoloration and ulcers may also occur. Recognizing these symptoms is vital for timely medical evaluation, promoting informed health decisions, and developing a comprehensive treatment plan. Proper recognition of these symptoms is essential to ensure a personalized and effective treatment approach.
Unveiling the Causes of CVI
Unveiling the causes of chronic venous insufficiency is crucial for tailoring treatment plans to individual needs. Factors such as venous reflux and vein valve dysfunction contribute to this condition. Additionally, a history of blood clots or vascular conditions may also play a role. Understanding these causes empowers individuals to take proactive steps in managing their condition and implementing preventive measures.
Progression of Chronic Venous Insufficiency
Understanding the advancement of CVI is crucial for timely intervention and preventing complications as it may evolve through stages, escalating symptoms and potential complications. Regular medical evaluations and monitoring are essential due to its progression. Timely intervention at each stage aids in preventing the development of venous ulcers, ultimately improving long-term outcomes and quality of life.
Stages of Chronic Venous Insufficiency
As chronic venous insufficiency progresses, symptoms like leg swelling and aching may appear, followed by pronounced skin changes, ulcers, and venous reflux. Staging CVI is crucial for targeted treatment strategies, highlighting the importance of early detection and prompt management. Healthcare providers use the stages of CVI to formulate effective treatment plans, emphasizing the need for timely intervention and personalized care.
The Most Common Cause of Chronic Venous Insufficiency
The primary cause of chronic venous insufficiency often stems from damaged or weakened vein valves, leading to blood accumulation in the lower extremities. Venous reflux, a condition where blood flows backward, and varicose veins are frequent culprits, contributing to venous insufficiency. Additionally, deep vein thrombosis and venous leg ulcers can also lead to the development of this condition.
Diagnosing Chronic Venous Insufficiency
When diagnosing chronic venous insufficiency, a medical history and physical exam are initial steps, considering symptoms, family history, lifestyle, and health conditions. Duplex ultrasound, a non-invasive test utilizing sound waves, visualizes affected veins and blood flow direction. Identifying skin changes like discoloration, ulcers, or swelling is crucial, indicating venous disorders and stasis ulcers. Assessing signs of venous insufficiency aids in diagnosing reflux, thrombosis, and venous disease, guiding treatment plans.
Understanding the Diagnostic Process for CVI
The diagnostic process for chronic venous insufficiency involves a thorough assessment, including a physical examination, medical history review, and the use of duplex ultrasound. It requires accurate identification of venous ulcers, varicose veins, and leg swelling, along with recognizing symptoms of venous reflux and venous disease. Detailed information on blood flow direction and vein wall conditions assists in understanding this diagnostic process.
Treatment Approaches for CVI
Early intervention through lifestyle adjustments, regular physical activity, and weight control can vastly enhance the lives of chronic venous insufficiency (CVI) patients, preventing severe swelling and venous ulcers. Compression therapy, a foundational CVI treatment, utilizes compression stockings to improve blood flow and reduce swelling. Minimally invasive procedures like laser therapy and chemical ablation provide effective options, while surgical treatments like vein stripping and radiofrequency ablation are reserved for severe cases. Medical management, including targeted medications, is integral to the treatment plan for affected individuals.
Available Treatments for CVI
When addressing chronic venous insufficiency, available treatments encompass compression therapy, lifestyle modifications, minimally invasive procedures, and surgical interventions customized to the condition’s severity. Compression stockings, elevating legs, laser therapy, and surgical options like vein stripping and radiofrequency ablation are part of a comprehensive treatment plan. These modalities aim to improve blood flow, prevent ulcers, and address larger vein issues.
Medical Management of CVI
Medical management of chronic venous insufficiency involves the use of medications, including blood thinners and anti-inflammatories, to address symptoms and blood clot risk. Proper wound care, such as topical treatments and dressings, is crucial for preventing infection and promoting healing. The main goal is to monitor and manage venous reflux, varicose veins, and deep vein thrombosis, supporting a comprehensive treatment approach.
Surgical Options for CVI
Exploring surgical options for chronic venous insufficiency involves procedures like vein stripping, radiofrequency ablation, and subfascial endoscopic perforator surgery. These interventions target severe cases, promoting healthy blood flow and reducing venous reflux. Vein bypass surgery creates an alternate route for blood flow, bypassing damaged veins to improve circulation in the lower extremities. Considering potential outcomes and recovery processes is crucial for both individuals and healthcare providers.
Preventing Chronic Venous Insufficiency
Weight management and regular exercise are crucial in preventing chronic venous insufficiency, reducing the risk of venous stasis ulcers and leg swelling. Lifestyle changes, such as elevating the legs and avoiding prolonged standing or sitting, play a key role. Understanding the risk factors, implementing proper leg care, and educating individuals are essential for prevention.
Risk Factors for Chronic Venous Insufficiency
Identifying risk factors for chronic venous insufficiency is crucial, including a family history, obesity, and deep vein thrombosis. Prolonged standing or sitting can impact blood flow and vein valves, while pregnancy-related changes and tobacco use can also play a role. Understanding these factors helps in identifying individuals at a higher risk, promoting early intervention and preventive measures.
Tips for Preventing CVI
To prevent CVI, engage in regular exercise like walking or swimming to promote healthy blood flow. Avoid prolonged standing or sitting to reduce the risk of venous reflux. Wear compression stockings to support vein valves and minimize blood pooling. Elevate your legs above the heart to improve blood flow. Implement lifestyle changes for proactive prevention.
Living with Chronic Venous Insufficiency
Chronic venous insufficiency can lead to leg swelling, skin changes, and venous ulcers. Compression therapy aids in improving blood flow and managing CVI symptoms. Lifestyle adjustments such as weight control and regular exercise, along with compression stockings, can alleviate CVI symptoms. Laser therapy and personalized medical guidance are also beneficial for treating chronic venous insufficiency.
Day-to-Day Management of CVI
To improve blood flow and reduce clotting, incorporate regular exercise into your routine. Alleviate CVI symptoms by wearing compression stockings and avoiding prolonged sitting or standing. Prevent skin changes and ulcers by moisturizing and protecting affected areas. Embrace a healthy lifestyle with balanced diet and weight management to manage CVI symptoms effectively.
Seeking Medical Help for CVI
Seeking appropriate medical attention is crucial if symptoms of CVI, including leg swelling, skin changes, and ulcers, persist. A vascular surgeon can conduct a comprehensive assessment using a physical exam, medical history review, and duplex ultrasound to diagnose and evaluate the severity of CVI. In severe cases, minimally invasive procedures like radiofrequency ablation may be recommended to address chronic venous insufficiency, supporting the main goal of managing its progression and preventing severe complications.
Can Chronic Venous Insufficiency be Cured Completely?
While complete cure for chronic venous insufficiency is not possible, symptoms can be effectively managed. Treatment focuses on improving quality of life, preventing complications, and reducing symptoms through personalized plans including lifestyle modifications and medical interventions. Long-term commitment to a healthy lifestyle and treatment plan is essential for managing CVI effectively.
Conclusion
In conclusion, chronic venous insufficiency (CVI) is a condition that affects many individuals and can have a significant impact on their health and well-being. It is crucial to understand the signs, causes, and progression of CVI in order to seek proper diagnosis and treatment. While there may not be a complete cure for CVI, there are various treatment approaches available, including medical management and surgical options, to help manage symptoms and improve quality of life. Additionally, taking preventive measures and seeking medical help when needed can also play a crucial role in living with CVI. Remember, it is important to prioritize your health and seek appropriate care for chronic venous insufficiency.